What is an ACL injury?
The anterior cruciate ligament (ACL) is a key structure in the knee joint kinematics, as it resists anterior tibial translation and rotational loads. The ACL provides approximately 85% of the total restraining force of anterior translation. It also prevents excessive tibial medial and lateral rotation, as well as varus and valgus stresses. Despite of that its primary role is a proprioceptive function due to the presence of mechanoreceptors in the ligaments. Because of that an ACL injury might therefore be regarded as a neurophysiological dysfunction and not as a simple peripheral musculoskeletal injury. As a consequence of its complex role in the kinematics of the knee, when an ACL injury occurs there are both clinical signs and subjective instability and therefore a comprehensive rehabilitation program is needed. Injuries to the ACL are relatively common knee injuries among athletes and females are two to eight times more likely to sustain an ACL injury than their male counterparts.
The injuries can range from mild (such as small tears/sprain) to severe (when the ligament is completely torn). When an ACL has a complete rupture and there are clinical and subjective signs of instability, a surgical reconstruction is needed. However it is not self-evident that an ACL Reconstruction will automatically lead to a return to preinjury activity level.
ACL rehabilitation is both for conservative and surgical option.
Clinically Relevant Anatomy
The anterior cruciate ligament (ACL) is a band of dense connective tissue which courses from the femur to the tibia. The ACL arises from the posteromedial corner of the medial aspect of the lateral femoral condyle in the intercondylar notch and inserted anterior to the intercondyloid eminence of the tibia, blending with the anterior horn of the medial meniscus. The ACL courses anteriorly, medially, and distally across the joint as it passes from the femur to the tibia. As it does, it turns on itself in a slight outward (lateral) spiral.
The density of blood vessels within the ligaments is not homogeneous. In the ACL, an avascular zone is located within the fibrocartilage of the anterior part where the ligament faces the anterior rim of the intercondylar fossa. The coincidence of poor vascularity and the presence of fibrocartilage is also seen in gliding tendons in areas that are subjected to compressive loads, plays a role in the poor healing potential of the ACL.
General Considerations
ACL rehabilitation has undergone considerable changes over the past decade. Intensive research into the biomechanics of the injured and the operated knee have led to a movement away from the techniques of the early 1980’s characterized by post operative casting, delayed weight bearing and limitation of Range of Motion (ROM), to the current early rehabilitation program with immediate training of ROM and weight bearing exercises.
The ACL rehabilitation is both for conservative and surgical options. Conservative treatment of an ACL injury could be the best choice for sedentary patients. Indeed, patient age, sportive activities and foremost subjective instability symptoms in daily life activities should be considered when deciding for or against ACL reconstruction. In those cases, a physiotherapic program of complete re-gain of ROM, a comprehensive program of reinforce and restore of proprioception and a normal gait pattern training could be the best rehabilitation protocol. However, if symptomatic instability of the knee is not reduced after physiotherapy nor after adjustment of activity, anterior cruciate ligament reconstruction is recommended. This might prevent multiple interventions because of further meniscal and cartilage damage.
It is useful to remember that injuries to the ACL rarely occur in isolation. The presence and extent of other injuries may affect the way in which the ACL injury is managed. Indeed, the mechanism of injury can damage also the Medial Collateral Ligament (MCL) or the meniscus. Other associated injuries could be microfractures or bone contusions, both with or without chondral injuries. In those cases, the ACL Rehabilitation program must be not standardized and consider the comorbidity.
The major goals of general rehabilitation of the ACL-injured knee:
- Gain full ROM of the knee
- Repair muscle strength and proprioception
- Gain in good functional stability
- Reach the best possible functional level (walking, running, jumping…)
- Decrease the risk for re-injury
- Return to sport
Acute Phase of ACL rehabilitation
After an ACL injury, regardless of whether surgery will take place or not, physiotherapy management focuses on regaining range of movement, strength, proprioception and stability. In the acute stage PEACE AND LOVE should be used in order to reduce swelling and pain, to attempt full range of motion and to decrease joint effusion. Appropriate anti-inflammatory medications are used to help control pain and swelling.
The indication of use crutches and eventually a knee immobilizer could be appropriate in some patients. However extended use of the knee immobilizer should be limited to avoid quadriceps atrophy.
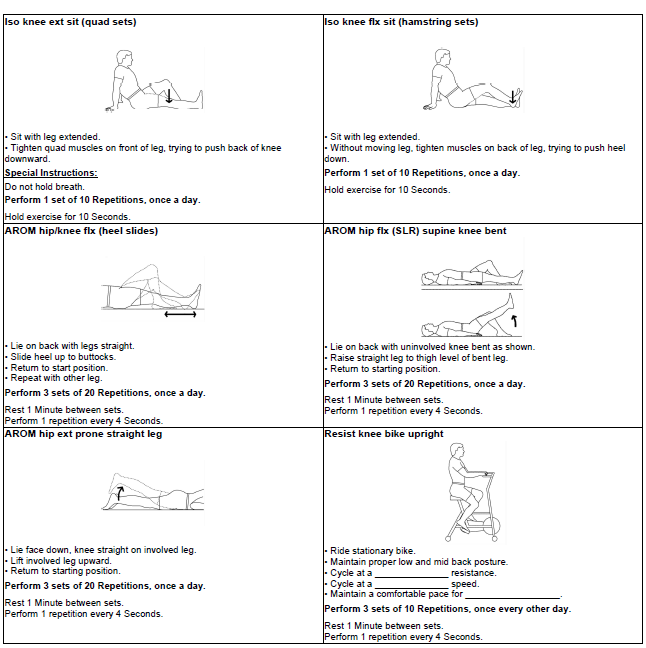
The neuro-muscular inhibition of the quadriceps caused by intrarticular effusion may have a negative effect on the strengthening. In any case exercises should encourage range of movement, initial strengthening of the quadriceps and hamstrings, and eventually proprioception. In fact, strength and proprioceptive alterations occur in both the injured and uninjured limb. To assist pre-operative optimization, the following guidelines are recommended in the acute and early sub-acute stages post injury:
- Full extension is obtained by doing:
- Passive knee extension: the physiotherapist can provide the passive knee extension both with manual therapy and teaching exercises adding leverage to gently force extension,
- Patellar self-mobilisations,
- Heel Props,
- Prone hang exercise,
- Static quads/SLR;
- Bending (Flexion) is obtained by doing:
- Passive knee bend: the physiotherapist can provide the passive knee flexion both with manual therapy and teaching exercises adding leverage to gently force flexion,
- Knee flexion in prone (gentle kicking exercises),
- Wall slides,
- Heel slides;
- Knee flexion/extension in sitting;
- Ankle DF/PF/circumduction;
- Glutes medius work in side lying;
- Gluteal exercises in prone;
- Weight transfers in standing (forwards/backwards, side/side).
It is also demonstrated that Neuromuscular Electrical Stimulation (NMES) combined with exercise is more effective in improving quadriceps strength than exercise alone.
It could be useful also to consider taping to provide stability and to encourage reduction in swelling.

